Can Montana’s Rural Nursing Homes Survive The Future?
While the solution — money — is simple enough, the problem is vexingly complex.
Almost overnight, most skilled-care facilities in Montana, which include nursing homes, went from getting by to now being on the brink of closure. Trade journals for the industry estimate small facilities with less than 100 beds are doomed, and for Montana and its rapidly graying population, that could spell a crisis in communities throughout the state.
Like so many things, the COVID-19 pandemic changed the way these facilities operate not just during lockdowns, but permanently. Wages for medical professionals spiked meteorically high, while the stress of the pandemic drove many professionals from the industry, creating high demand and even higher wages. Valley View Home in Glasgow, a facility that handles about 75 patients, saw the cost of nursing staff double almost overnight as nurses fled to companies contracting for traveling nurses. Nurses had been aided by national standards that allowed them to travel across state lines without needing additional licensing, a nod to the pandemic protocols that left the industry scrambling for trained medical professionals.
Alissa Kuka, director of nursing at Valley View, said that nurses walked out to take the higher paying jobs, often doubling their salaries overnight. That left skilled nursing facilities in a constant crisis of staffing shortage all while dealing with the pandemic.
Only last month has Valley View Home received its first employment application in nearly two years.
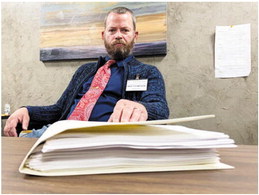
Wes Thompson, the administrator of Valley View, said nursing costs of the Valley County facility consume about 90 percent of the budget, so when the wages doubled, the facility went from having its best year in recent history to teetering on the brink of financial implosion. This fall, Thompson said, the community will vote on renewing the tax district that helps support the facility that has had to cut back on virtually any admission of a resident who isn’t a county resident. Without that support, the facility wouldn’t be able to operate. But with rising costs, diminishing government support and demand far outpacing the supply, Valley View’s future is, by Thompson’s own account, quarter-to-quarter.
Duane Murray, the administrator of Hi-Line Retirement Community in Malta, just one county over, echoes the same concerns. In addition to being the administrator and director of nursing for the 56-person facility, he also takes some shifts as a registered nurse.
Murray came out of retirement to help save the facility that employs 50 people. Just two years ago, that number was 70. He’d hire more people, but there’s no one to hire.
Money also factors in the health of these organizations. While inflation and wage costs have been extreme, the reimbursement system is also fundamentally broken.
For example, most of the long-term residents who rely on nursing homes are Medicaid patients. However, the reimbursement level doesn’t cover the full cost of providing the housing, care and staff. That means residents who have private insurance subsidize others’, but often private-pay residents have the financial means to care for themselves or buy in-home help. Usually, if a private-pay patient comes to one of the skilled-nursing facilities, it’s just for a brief time to rehabilitate or toward the end of life.
This leaves a business model in which the bulk of the residents represent a loss.
Paperwork that has to be filed, even to care for more critically complex clients, often takes weeks, if not months, for reimbursement. For example, recently, Thompson and his staff had to file extra paperwork for reimbursement for 16 residents in one month. It took seven months for the reimbursement check to come back.
“We have priced ourselves out,” Murray said.
By keeping costs so low, and not reflecting the true amount it takes to operate facilities, the alarm bells are way past due, he said.
“People don’t realize how expensive it is, and it’s not politically correct to make money off of Medicare,” he said.
Other problems, like onerous regulations and rules that haven’t seemed to quite catch up with the times, seem to plague industry. For example, Murray pointed out that Medicaid does not pay for assisted living, meaning that those facilities, which may be more appropriate for residents, are skipped in favor of the more costly skilled nursing facilities.
Warm Springs
Rural leaders have watched from miles away as lawmakers and state officials struggle to keep the state’s hospital in Warm Springs open. A combination of complex cases, low staff morale, high turnover, chronic underfunding and a rural location have conspired to lead to a loss of federal Medicaid payments to the institution, resulting in the facility hemorrhaging state money.
State officials said funding the facility takes a lot more than the $600 per day per patient currently budgeted. However, health care leaders like Thompson and Murray are incredulous. The state allocates $600 per day for Warm Springs, but statewide, only about $211 a day for other residents in skilled nursing facilities.
“If they can’t make it at $600 per day, how are we supposed to make ends meet at $200?” Thompson said.
Even though contract nursing, which became so utilized during the COVID-19 pandemic, has seen rates decline, it’s still much more expensive than when the disease started in 2020. Thompson said the rates for contract nurses can run between $320 and $400 per day.
Kuka lost many nurses to the travel nursing model and high per diem rates.
“The rate isn’t going back down to anywhere sustainable,” Kuka said. In 2019, Kuka said Valley View had no contract nursing. At one point during the past two years, that number climbed to nearly 68 percent, but has since receded.
Kuka said that even within the nursing industry, many nurses want to be in highly specialized areas, like the emergency department of a hospital or on a labor-and-delivery, not in a skilled nursing facility.
“There’s a stigma about it,” said Murray, who is also a registered nurse. “All nurses seem to migrate to a hospital, and it’s not as medically sexy.”
Kuka said one skilled nursing facility in Darby is sitting on a $25,000 sign-on bonus for a nurse willing to stay on long enough to claim the cash bounty after a year’s worth of work.
Murray has run the math. He figures the cost of regulations to make sure his Malta facility is in compliance with state and federal law can run as much as $3,000 per resident per month.
Murray and Thompson credit state Sen. Mike Lang, R-Malta, with facilitating meetings between Helena and leaders in the rural areas.
“Personally, I think we’re so concerned with what’s happening at the state hospital and the charges and the contract labor, but it’s the same as what is happening at every other facility in the state,” Lang said.
When lawmakers first devised the reimbursement system for skilled nursing facilities, Thompson said the model worked, but it hasn’t been revisited substantially. For example, the federal government pays two-thirds of all Medicaid, so there’s no incentive to cut the state spending because for every dollar that’s cut from the state, two more federal dollars comes out the economy.
However, when the model was implemented, Medicaid in nursing homes only accounted for 65% of all patients. The rest was comprised of private-pay patients. Thompson said this ratio was just enough to make it financially viable by charging private- pay clients more. Now, in some facilities, Medicaid patients make up as much as 90 percent of the clients, tilting the economic formula toward disaster.
“In my time in the industry, private pay has dwindled for at least 20 years, but costs are still going up,” Murray said. The Donut-Hole Challenge
The problem also seems to strains rural facilities of medium size by Montana standards. Often, larger corporations and for-profit businesses are attracted to skilled nursing facilities in Montana’s seven largest cities. The abundance of clients and labor, plus being closer to other medical facilities, often mean those facilities will survive the twists and turns of an uncertain labor market and a pandemic.
Smaller communities, on the other hand, use a “swing bed” model that helps facilities keep afloat. The model allows facilities in the smallest communities with fewer than 25 beds to keep a number of permanent residents in skilled nursing, then use a remaining number as “swing beds,” often for those with minor illnesses or recovering from surgery. This model allows these smaller facilities to use the same staff and facilities to care for temporary patients as well as longer- term residents. Yet the “donut hole” exists when facilities, like those in Glasgow and Malta, are located in communities large enough not to use a “swing bed” model but too small to be part of a larger health care business.
“In my mind, the only thing to save us is the same kind of model like a critical access hospital where there are different rules,” Thompson said.
The critical access hospital model uses a different kind of reimbursement rate for rural hospitals than for larger ones. For example, in an effort to keep a robust network of small hospitals in rural communities, reimbursements are calculated differently, helping to cover more costs.
“Theoretically, the smalltown hospitals can’t lose money,” Murray said.
But there’s no such protection for skilled nursing facilities, even though many rural towns expect a nursing home, along with a hospital or a doctor’s clinic.
Sen. Lang said many rules and regulations, written by the federal government, are also incredibly costly for smaller facilities, adding to an already stretched bottom line. In other words, larger facilities have economies of scale when it comes to filing reports and complying with requirements, but in smaller communities, the same job of reporting is required of the smaller staff.
Attorney Matt Knierim, who works with the skilled nursing facilities, said it may be a mindset problem with the state and lawmakers. For example, the GOP-led Legislature likes to talk about economic development and infrastructure.
“In that conversation, hospitals and nursing homes get shoved aside,” Knierim said. “But the No. 1 recruiting problem usually centers around bringing someone to a community, and they want to know if they can gave a baby there, or will they have to drive somewhere else? Or, if they’re taking care of a loved one, they want to know if there’s a place for mom, or will they have to go to Great Falls or Billings?
“They look for co-services, so when you’re talking about jobs and recruiting, you have to look at your long-term medical care along with all the other community services.”
Murray and Thompson believe one of the possibilities to saving skilled nursing facilities is by the state encouraging more collaboration and partnership with hospitals.
“Hospitals have to get on board because we are an extension of them,” Murray said.
When patients are discharged, often they need a short- or long-term stay at a skilled nursing facility. However, Thompson said nearly all the residents in Glasgow are in-county residents. That leaves discharge planners in hospitals around the state with a similar problem: Where do patients go?
The Patient Problem
As America and Montana grow more gray, more than half of the residents who need skilled nursing care suffer from some form of dementia. But memory care and dementia care can require more staffing and more management. And as America’s waistlines also grow, more people needing care require special beds and lifts for safety, something that not every facility has or can afford. Knowing how to care for larger, heavier patients is not just a matter of patient safety, but staff safety, too.
“None of us can accept some of these patients because of safety needs,” Thompson said.
This means that for family looking to bring loved ones closer to home in places like Phillips County, the closest facility may be hours away.
Kuka said that the average profile of a resident is also changing. For example, four years ago, the average new resident of the facility was more than 85 years old. Today, that number is dropping dramatically. They’re becoming younger and sicker. Heart disease, diabetes, mental health disorders and substance abuse are all reasons why someone may need skilled nursing facilities.
“We are talking about people who really abused their bodies,” Kuka said. “Now, we’re frequently seeing patients in their 40s and 50s, and they’re a whole different ballgame.”
Most of the skilled care facilities were also built with a double-occupancy model. That helped drive efficiency, but it has almost all but disappeared.
“Our generation has higher expectations, and there’s a reason why no one has built a skilled nursing facility recently,” Murray said. “No one wants double occupancy, and so many of these facilities have half the beds than they were planned for.”
Like It’s 2019
To demonstrate the longterm effects of the pandemic, Thompson points to the bottom line of the Glasgow skilled-nursing facility. In 2019, it posted its financials with the best year since 2003, and it reported positive cash flow.
With 90 cents on every dollar going to people, the majority of expenses in skilled nursing facilities are staffing. The year 2020 marked the rise of traveling health professionals, and the facility went from financially stable to, at best, uncertain.
Thompson knows what his obligations are to the residents. And that’s just as ominous as it sounds. He knows, for example, that he would want to give most a six-month notice about closing — something he hopes to avoid, literally at all costs.
But since 2019, he’s moved from thinking strategically about the home’s future in three years to the question: What happens if nothing changes?
“That’s not a question for anytime in the near future, but if things don’t change in the next six months to one year, what do we do?” he asked.
Valley County is considering supporting the Glasgow facility through a levy. If that is renewed, it will help, but Thompson said they simply cannot tax enough to keep the doors open, let alone put money away for emergencies. And like most skilled nursing facilities throughout the state, the building was constructed in the 1970s, so its age is showing, but Medicaid and even the more lucrative private pay insurers don’t cover costs like that.
“This business model is broken,” Knierim said.
Murray put it a different way for his Malta facility. It has $4 million in debt and the facility is appraised at $2.6 million.
“There’s no corporation going to come to Malta,” Murray said. “The only other people besides CEOs or nurses that are begging for any support or the ones to start screaming and hollering are family members. But even they don’t care about a nursing home until they need it.”


